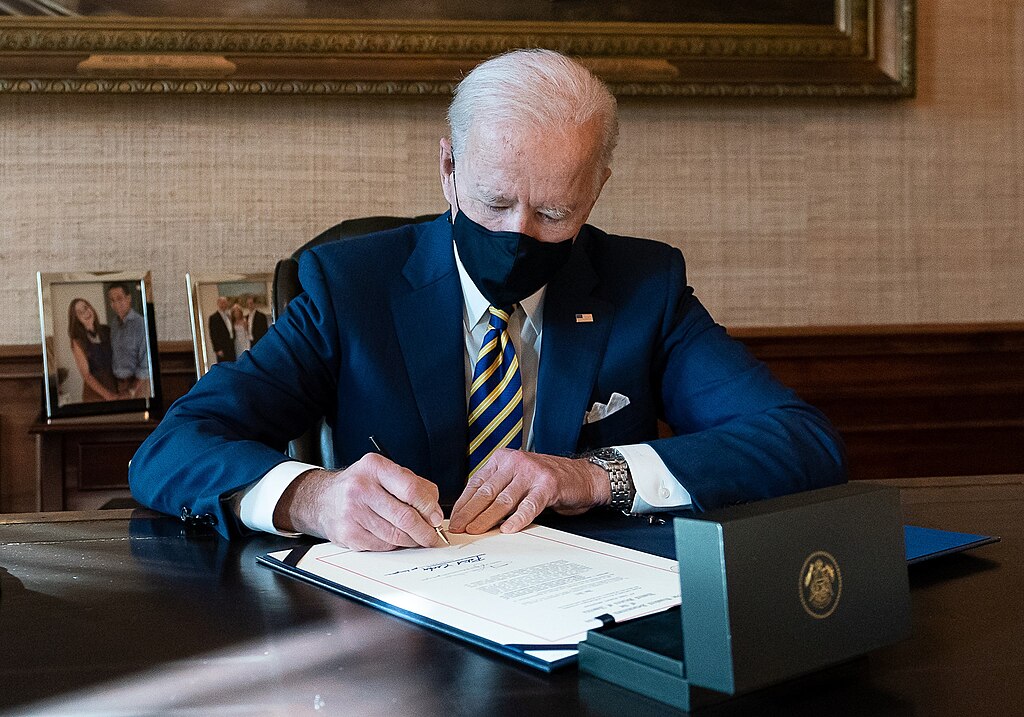
In a landmark decision aimed at addressing the nationwide organ shortage, the Biden administration announced a new rule on Tuesday permitting organ transplants between HIV-positive donors and HIV-positive recipients. U.S. health officials revealed that the policy, which takes effect Wednesday, seeks to expand the organ donor pool and shorten waiting times for all patients requiring transplants, regardless of HIV status.
The groundbreaking change removes long-standing barriers, as such transplants were previously confined to research studies. U.S. Health and Human Services (HHS) Secretary Xavier Becerra lauded the move, stating it would "improve outcomes for transplant recipients with HIV while bolstering the donor pool."
Understanding HIV and the Challenges of Treatment
Human immunodeficiency virus (HIV) compromises the immune system by attacking CD4 cells, leaving the body vulnerable to infections and diseases. While modern treatments, such as combination antiretroviral therapy (cART), have significantly improved the quality of life for those with HIV, there is no definitive cure. Over 1.2 million Americans currently live with HIV, and approximately 30,000 new cases are diagnosed annually.
The goal of cART is to suppress the virus to undetectable levels in the bloodstream, enabling the immune system to recover and reducing the likelihood of HIV progressing to AIDS. However, the virus can remain dormant in the body, posing ongoing challenges. Despite these complexities, advancements in medicine have made organ transplantation between HIV-positive individuals a viable and safe option.
Research Supporting the Rule
The Biden administration’s decision is rooted in extensive research demonstrating the safety and efficacy of HIV-positive organ transplants. A study published in the New England Journal of Medicine tracked nearly 200 transplant recipients over four years, comparing outcomes between those receiving organs from HIV-positive and HIV-negative donors. The results indicated similar survival rates and low rejection risks across both groups.
The precedent for HIV-positive transplants dates back to 2010 when South African surgeons performed successful procedures using organs from HIV-positive donors. In the U.S., restrictions were initially lifted in 2013 for research purposes, culminating in a milestone in 2019 when Johns Hopkins University completed the world’s first kidney transplant between a living HIV-positive donor and an HIV-positive recipient. Since then, over 500 similar transplants have been conducted across the country, with experts heralding the practice as a critical step forward in medical innovation.
Reactions and Implications
The new rule has been widely celebrated by advocates for HIV-positive individuals and public health experts, who view it as a long-overdue measure to alleviate the critical shortage of donor organs. However, it has also ignited spirited debate online.
- @HIVAdvocate123: "This is a win for public health and those living with HIV. Progress at its finest!"
- @TransplantTruths: "Finally, a policy that puts science first! This will save lives and break unnecessary barriers."
- @HealthCritic99: "Great move, but what about ensuring proper care post-transplant for recipients?"
- @OrganDonorAdvocacy: "HIV-positive donors are heroes! Let’s celebrate this historic step in medicine."
- @SkepticVoice: "More education is needed about this process. Not everyone understands what this means for organ shortages."
- @PositiveLivingUSA: "Hope for so many who’ve waited too long. Biden administration deserves credit for pushing this forward."
A Leap for Medical Progress
This decision, backed by years of research and successful implementation in clinical settings, is expected to provide new hope for individuals living with HIV while easing the strain on the broader transplant system. By expanding the pool of eligible donors, the Biden administration aims to tackle the growing demand for life-saving organs and advance public health on multiple fronts.



 Trump Announces U.S. Strikes on Iran Navy as Conflict Escalates
Trump Announces U.S. Strikes on Iran Navy as Conflict Escalates  Israel Declares State of Emergency as Iran Launches Missile Attacks
Israel Declares State of Emergency as Iran Launches Missile Attacks  Iran Supreme Leader Ayatollah Ali Khamenei Killed in Israeli, U.S. Strikes: Reuters
Iran Supreme Leader Ayatollah Ali Khamenei Killed in Israeli, U.S. Strikes: Reuters  Russia Signals Openness to U.S. Security Guarantees for Ukraine at Geneva Peace Talks
Russia Signals Openness to U.S. Security Guarantees for Ukraine at Geneva Peace Talks  HHS Adds New Members to Vaccine Advisory Panel Amid Legal and Market Uncertainty
HHS Adds New Members to Vaccine Advisory Panel Amid Legal and Market Uncertainty  Federal Judge Orders Trump Administration to Facilitate Return of Deported Honduran Student
Federal Judge Orders Trump Administration to Facilitate Return of Deported Honduran Student  Netanyahu Suggests Iran’s Supreme Leader Khamenei May Have Been Killed in Israeli-U.S. Strikes
Netanyahu Suggests Iran’s Supreme Leader Khamenei May Have Been Killed in Israeli-U.S. Strikes  Trump Orders Federal Agencies to Halt Use of Anthropic AI Technology
Trump Orders Federal Agencies to Halt Use of Anthropic AI Technology  Germany and China Reaffirm Open Trade and Strategic Partnership in Landmark Beijing Visit
Germany and China Reaffirm Open Trade and Strategic Partnership in Landmark Beijing Visit  Supreme Court Reviews Trump Administration Policies on Tariffs, Immigration, and Federal Power
Supreme Court Reviews Trump Administration Policies on Tariffs, Immigration, and Federal Power  Panama Cancels CK Hutchison Port Contracts, Grants Temporary Control to Maersk and MSC
Panama Cancels CK Hutchison Port Contracts, Grants Temporary Control to Maersk and MSC  Zelenskiy Urges Change in Iran After U.S. and Israeli Strikes, Cites Drone Support for Russia
Zelenskiy Urges Change in Iran After U.S. and Israeli Strikes, Cites Drone Support for Russia  Macron Urges Emergency UN Security Council Meeting as US-Israel Strikes on Iran Escalate Middle East Tensions
Macron Urges Emergency UN Security Council Meeting as US-Israel Strikes on Iran Escalate Middle East Tensions  California Seeks Court Order to Halt Amazon’s Alleged Price Inflation Practices
California Seeks Court Order to Halt Amazon’s Alleged Price Inflation Practices  Federal Court Fines Mobil Oil Australia A$16 Million for Misleading Fuel Claims
Federal Court Fines Mobil Oil Australia A$16 Million for Misleading Fuel Claims  Medical Groups Sue FTC Over Gender-Affirming Care Investigations Amid Trump Policy Dispute
Medical Groups Sue FTC Over Gender-Affirming Care Investigations Amid Trump Policy Dispute  FedEx Faces Class Action Lawsuit Over Tariff Refunds After Supreme Court Ruling
FedEx Faces Class Action Lawsuit Over Tariff Refunds After Supreme Court Ruling