A man – for the sake of this exercise, let’s call him “Paul” - has a heart attack and his brain is starved of oxygen. After several resuscitations and a week in a coma, he finally opens his eyes. However, he doesn’t always appear to be present. Doctors say he is still unconscious, in an “unresponsive state” – the patient’s eyes are open, but he doesn’t move his hand when asked. For families in such situations, the question is always the same: will their loved one become conscious again?
Recent advances in intensive-care medicine have allowed many people with severe brain injuries to “come back to life”. However, from a seemingly inert state to full wakefulness, there is a wide range of different states of consciousness that neuroscientists are working to better define.
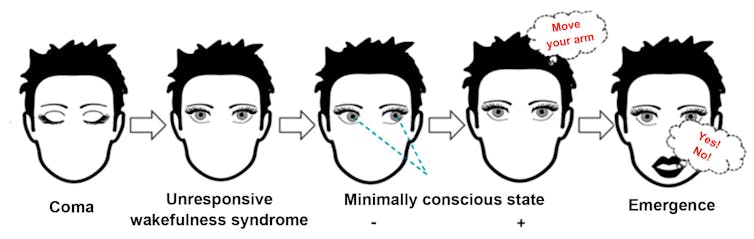
After a coma episode (where the eyes remain closed) lasting between one hour and four weeks, there are normally several states of recovery until “emergence”, but some intermediate states of consciousness may persist and even become chronic:
-
Unresponsive wakefulness syndrome: the patients open their eyes but show no signs of consciousness. (This was previously called a “vegetative state”, but was renamed in 2010 to better describe the symptoms.)
-
Minimally conscious state “minus”: recovery of some signs of consciousness such as visual pursuit/fixation, or localization of painful stimulation.
-
Minimally conscious state “plus”: reappearance of signs of language awareness – response to verbal commands, production of words, attempts to communicate.
-
Emergence from the minimally conscious state: as soon as the patient is able to communicate using a yes/no code or to use everyday objects.
Diagnosis of the state of consciousness following brain damage: coma, unresponsive wakefulness syndrome (vegetative state), minimally conscious state minus, minimally conscious state plus and emergence. Wislowska et al. (2017). Night and day variations of sleep in patients with disorders of consciousness
It is crucial to be able to distinguish these disorders of consciousness from a locked-in syndrome, also the result of a severe brain injury, but located in the brain stem. The result is paralysis of the body, head and face, although consciousness and cognition may be preserved. Communication is most often achieved through eye movements.
The challenging diagnosis of disorders of consciousness
Such altered states of consciousness are difficult to diagnose because brain imaging does not yet allow an optimal diagnosis of unresponsive wakefulness or minimal consciousness. The most widely accepted method at present is a bedside assessment using standardized and validated scales. The Glasgow Coma Scale is the most known and investigated one. However, it does not assess the most frequent signs of minimal consciousness (notably visual fixation/pursuit). This is in contrast to the Coma Recovery Scale-Revised or the Simplified evaluation of consciousness disorders, which identify auditory, visual, motor and language signs of consciousness.
Without such assessments, a diagnosis based on simple clinical observation would have about 40% error. These assessments must be repeated about five times in a short period of time (for example, two weeks), reducing the risk of diagnostic errors from 36% after one assessment to 5% after the fifth.
The challenge in making a correct diagnosis on the basis of behavioural assessments is partly related to patients’ fluctuating level of arousal, and also lesions such as palpebral ptosis – inability to open the eyes – that can impede the assessment of visual fixations/pursuits.
A new approach through language
One of the most frequent questions health professionals are faced with when taking care of these patients is: “Can they understand us?” The assessment of language skills is also a key step in establishing communication with the patient. However, if the language regions of the patient’s brain have been too damaged, their state of consciousness could be underestimated – he or she may not respond to commands simply because they’re not understood. Indeed, a 2015 study of stroke patients with aphasia – language impairment following brain damage – showed that about 25% of who were fully conscious could be erroneously diagnosed as minimally conscious.
These data underline the importance of improving the assessment of language in patients waking up from coma. Current research is trying to better understand how we can assess the language abilities of these patients, despite their visual, auditory and motor dysfunctions.
An aid to limit misdiagnosis
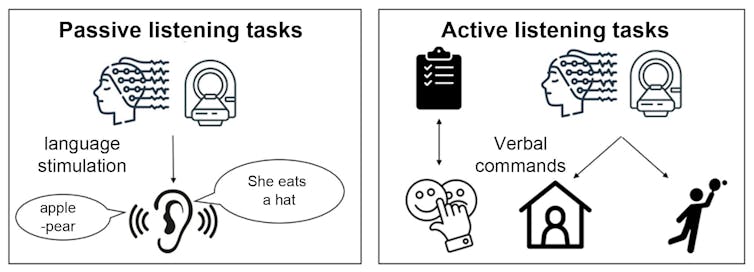
Our recent systematic review of the literature reports the use of electroencephalography (EEG) or magnetic resonance imaging (MRI) methods, which make it possible to measure the activity of brain regions generally linked to language. Two types of tasks can be performed with either technique:
-
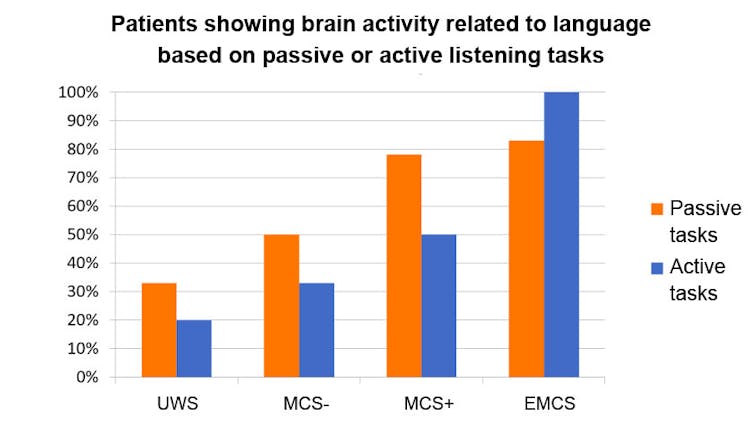
Passive listening tasks consist of having patients listen to words or sentences. For example, we look at the difference in brain activity depending on whether the patient hears noise or language. According to the studies reviewed, about 33% of patients considered to have an unresponsive wakefulness syndrome show signs of language comprehension.
-
Active listening tasks, in which the patient is asked to think about a physical activity – for example, “Imagine playing tennis”. If the patient shows signs of the activation of motor imagery on EEG or MRI, it can be deduced that he or she has responded to the command. Approximately 20% of patients considered to have an unresponsive wakefulness syndrome are able to perform these tasks.
Passive vs. active tasks to identify language comprehension in awake coma patients. The former are based on EEG and MRI and assess brain activity in response to different language stimuli; the latter measure the ability to respond to verbal commands, either behaviourally or via EEG and MRI. Charlène Aubinet
The level of consciousness of these patients could therefore be misdiagnosed. Since they respond to commands, they are actually in a minimally conscious state.
The consequences of misdiagnosis
Such diagnostic errors can have a significant impact on the prognosis and management of the patient. This is because health care staff tend to be more attentive to the pain management of a minimally conscious patient than an unresponsive patient who is considered to have impaired pain perception. More importantly, end-of-life decisions will be discussed more often in the case of an unresponsive patient.
One-third and one-fifth of patients with an unresponsive wakefulness syndrome (UWS) respond to passive and active tasks, respectively. As their level of consciousness increases, through the minimally conscious state (MCS) and up to the emergence from the minimally conscious state (EMCS), more residual language abilities are observed in patients. Charlène Aubinet
It therefore seems crucial to improve language assessment to better capture coma patients’ actual state of consciousness. Such efforts are only precipitated by the fact health professionals do not always have access to EEG and MRI techniques. At Liège University, our team has developed a “brief evaluation of receptive aphasia” (BERA) tool that presents pairs of images to the patient, prompting them to fix their eyes on the one that corresponds to the word or sentence they hear. With this test, we hope to provide a new, easily accessible and inexpensive tool for all clinicians in coma recovery.
There are still many advances to be made in this area of clinical research. The methods of assessment (but also of rehabilitation) will have to evolve in parallel with those of intensive care medicine, in order to help patients such as “Paul” to be able to communicate again.
For health professionals wishing to learn more, online materials are available on our [new diagnostic scales].



 Weight-Loss Drug Ads Take Over the Super Bowl as Pharma Embraces Direct-to-Consumer Marketing
Weight-Loss Drug Ads Take Over the Super Bowl as Pharma Embraces Direct-to-Consumer Marketing  Federal Appeals Court Blocks Trump-Era Hospital Drug Rebate Plan
Federal Appeals Court Blocks Trump-Era Hospital Drug Rebate Plan  Sanofi to Acquire Dynavax in $2.2 Billion Deal to Strengthen Vaccine Portfolio
Sanofi to Acquire Dynavax in $2.2 Billion Deal to Strengthen Vaccine Portfolio  Novo Nordisk Warns of Profit Decline as Wegovy Faces U.S. Price Pressure and Rising Competition
Novo Nordisk Warns of Profit Decline as Wegovy Faces U.S. Price Pressure and Rising Competition  FDA Approves Mitapivat for Anemia in Thalassemia Patients
FDA Approves Mitapivat for Anemia in Thalassemia Patients  TrumpRx.gov Highlights GLP-1 Drug Discounts but Offers Limited Savings for Most Americans
TrumpRx.gov Highlights GLP-1 Drug Discounts but Offers Limited Savings for Most Americans  RFK Jr. Overhauls Federal Autism Panel, Sparking Medical Community Backlash
RFK Jr. Overhauls Federal Autism Panel, Sparking Medical Community Backlash  AstraZeneca’s LATIFY Phase III Trial of Ceralasertib Misses Primary Endpoint in Lung Cancer Study
AstraZeneca’s LATIFY Phase III Trial of Ceralasertib Misses Primary Endpoint in Lung Cancer Study  Viking Therapeutics Sees Growing Strategic Interest in $150 Billion Weight-Loss Drug Market
Viking Therapeutics Sees Growing Strategic Interest in $150 Billion Weight-Loss Drug Market  Sanofi’s Efdoralprin Alfa Gains EMA Orphan Status for Rare Lung Disease
Sanofi’s Efdoralprin Alfa Gains EMA Orphan Status for Rare Lung Disease  Merck Raises Growth Outlook, Targets $70 Billion Revenue From New Drugs by Mid-2030s
Merck Raises Growth Outlook, Targets $70 Billion Revenue From New Drugs by Mid-2030s  Novo Nordisk and Eli Lilly Cut Obesity Drug Prices in China as Competition Intensifies
Novo Nordisk and Eli Lilly Cut Obesity Drug Prices in China as Competition Intensifies